Carol Peng, MD Kashif Munir, MD @CCPeng98 @ummidtownim #HualienTzuChiHospital #AtrialFibrillation #Cardiology #Resear...
Carol Chiung-Hui Peng, MD from the University of Maryland Medical Center Midtown Campus, and Kashif Munir, MD from the University of Maryland School of Medicine, associate professor, and Medical Director of the University of Maryland Center for Diabetes and Endocrinology speak about Non‐vitamin K antagonist oral anticoagulants vs. warfarin for AFib patients: What the latest research tells us.
Twitter -
@UMMC @umms @UMmedschool
Link to Abstract:
https://dom-pubs.onlinelibrary.wiley.com/doi/10.1111/dom.14243
Abstract
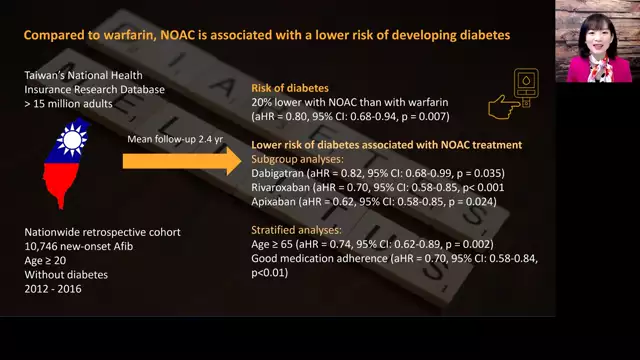
Comparison of the risk of developing diabetes in patients with non-vitamin K antagonist oral anticoagulants (NOACs) treated with atrial fibrillation (AF) and warfarin.
Materials and Methods
Using Taiwan's National Health Insurance Research Database, we carried out a nationwide retrospective cohort analysis. Adult new-onset AF patients treated with NOACs or warfarin between 2012 and 2016 have been included. The NOAC cohort was further categorized into classes of dabigatran, rivaroxaban, and apixaban. Incident diabetes requiring treatment with antidiabetic medications was the primary outcome. Subdistribution hazard models of Fine and Gray were used to estimate the adjusted hazard ratio (aHR). For each head-to-head analysis, propensity score matching was conducted.
Outcomes
Our analysis included a total of 10,746 new-onset AF patients. NOACs were associated with a lower risk of developing diabetes than warfarin during the mean 2.4-year follow-up (aHR = 0.80, 95 percent confidence interval [CI]: 0.68-0.94, P = .007). Analyses of the subgroup indicated that dabigatran, rivaroxaban, and apixaban each had a decreased risk of diabetes. Stratified studies found that the lower risk of NOAC-related diabetes was specific for patients 65 years of age or older (aHR = 0.74, 95% CI: 0.62-0.89, P = .002) and those with strong adherence to medication (aHR = 0.70, 95% CI: 0.58-0.84, P < .001).
Findings
In patients with AF, taking NOAC was associated with a lower risk of developing diabetes compared to taking warfarin.