Dr. John A. Bittl, MD- Putting the 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization Into Practice @B...
In 1997, Dr. Bittl joined Dr. Feldman's staff at the MRMC Cath Lab (now AdventHealth Ocala). He graduated from Johns Hopkins University in Baltimore, Maryland, with a medical degree. He did his residency and cardiology fellowship at UCLA Hospital in Los Angeles, CA, and Brigham and Women's Hospital in Boston, MA. Dr. Bittl also worked as an associate professor of medicine at Harvard Medical School. In this video Dr. Bittl speaks on Putting the 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization Into Practice: A Case Series.
https://www.jacc.org/doi/10.1016/j.jaccas.2021.09.025
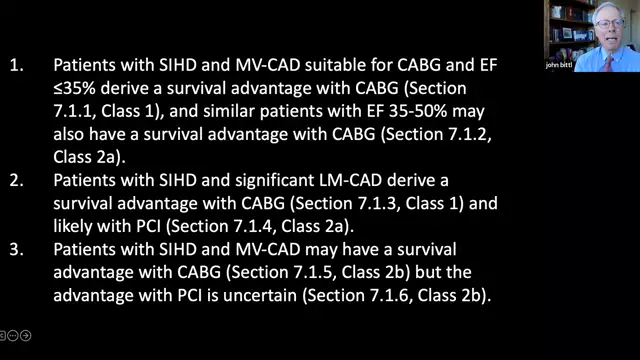
In selected subsets of patients with stable ischemic heart disease and complex coronary disease with or without left ventricular dysfunction, the 2021 ACC/AHA/SCAI guideline for coronary artery revascularization can be used to decide between revascularization and optimal medical therapy to reduce mortality or cardiovascular events. (Advanced level of difficulty.)
Introduction
The ISCHEMIA (International Study of Comparative Health Effectiveness with Medical and Invasive Approaches) (1) trial debunked the conventional wisdom that routine revascularization with either coronary artery bypass graft (CABG) surgery or percutaneous coronary intervention (PCI) improves survival in patients with multivessel (MV) coronary artery disease (CAD) and stable ischemic heart disease (SIHD), a belief that was based on the findings of several early studies and was supported by (2). The ACC/AHA/SCAI guideline drafting committee for coronary artery revascularization in 2021 (3) has analyzed the results of the new trial (1) against the background of existing evidence to identify patient subsets likely to benefit from revascularization in terms of survival. The following case series demonstrates how doctors can utilize the 2021 guideline (3) to assess which patients with SIHD may benefit from revascularization over medical therapy (MT) alone in terms of survival or cardiovascular events.