Mads Hashiba Jensen, med.stud @MadsHashiba @uni-copenhagen @UCPH_Health @koebenhavns_uni #Atrial Fibrillation #SleepA...
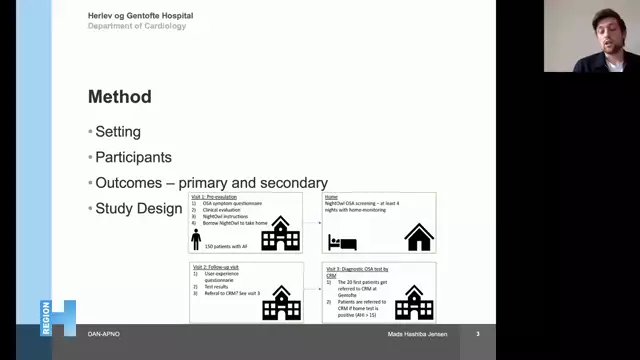
Mads Hashiba Jensen, a Medical Student at the Department of Cardiology at Herlev og Gentofle Hospital and the University of Copenhagen a presentation on DANish Patients With Atrial Fibrillation and Sleep Apnea Prevalence by Night Owl (DANAPNO).
Link to Study:
https://www.clinicaltrials.gov/ct2/show/NCT04760002?term=04760002&draw=2&rank=1
Description of the Research -
A study to see whether NightOwl could be used to detect the prevalence of obstructive sleep apnea (OSA) in patients with atrial fibrillation (AF). The long-term goal is to use the system to test for OSA in AF patients undergoing ablation and/or AF patients undergoing cardioversion in a randomized clinical trial.
Patients with some form of AF who are referred to a nurse-run ambulatory for anticoagulation initiation will be required to participate. The ambulatory consists of four regular nurse-led tracks at Herlev-Gentofte University Hospital's Department of Cardiology. In a formal partnership, Herlev-Gentofte University Hospital's Department of Pulmonology offers work-up with cardio-respiratory monitoring investigation and clinical assessment of starting sleep apnea care in patients referred from the study. Those in attendance Participants will be recruited from the Thrombosis unit (Tromboseklinikken) at Herlev-GentofteHospital who have AF without established sleep apnea and a need for anticoagulation. As part of their routine check at the anticoagulation outpatient clinic at Herlev and Gentofte Hospital, participants will be contacted and invited to participate in the research project by a local investigator or a project nurse. Participants will be given verbal details about the research project as well as the appropriate time to discuss recruitment during the interview. The written participant information will be given to the participants before the verbal information, and it will be given to them by a researcher or a project nurse who is well-versed in the project. Before a written informed consent is received, the investigators will be given the details they need to find eligible participants. The written informed consent enables the researchers to access the participant's medical health records for the purposes of the study.
The analysis is cross-sectional in nature. A third visit will be scheduled for the first 20 participants and those with an apnea-hypopnea index (AHI)>15 who are included in the sample.
The participant borrows a NightOwl and receives system guidance during the initial visit, which includes a clinical assessment and a questionnaire about OSA symptoms.
In a home setting, NightOwlTM was used for four nights of recording.
A follow-up visit to discuss the findings of the home surveillance and the soft node questionnaire.
A fourth visit to the sleep apnea clinic will be scheduled for the first 20 patients, as well as all patients whose home test shows (AHI>15).
The research will take about 6 months from the time the first patient is enrolled until the last patient is enrolled.

![Atrial Fibrillation SOC: An Electrophysiologist Review [2022] Atrial Fibrillation SOC: An Electrophysiologist Review [2022]](https://cardiologytalk.com/videos/video_221020224639_vd1ff/video_221020224639_vd1ff.webp?cache=1666306004_1666306004)