JACC: CardioOncology Virtual Journal Club - June 30, 2020
Editor-in-Chief Dr. Bonnie Ky hosts the inaugural JACC: CardioOncology Virtual Journal Club. Feature presentations include manuscripts from the Journal’s June 16 issue, followed by panelist discussion and questions from audience members. Learn more on JACC.org: https://tinyurl.com/ycj8skds
17 Views
3 years Ago
Cardio-Oncology
Description
Cardio-Oncology
Joshua D. Mitchell, MD- @JoshMitchellMD @Dr_Daniel_Cehic @CarmenBergom @ICOSociety #CardioONC #CardioOncology #Cardio...
Joshua D. Mitchell, MD- @JoshMitchellMD @Dr_Daniel_Cehic @CarmenBergom @ICOSociety #CardioONC #CardioOncology #Cardio...
Stefan Janssens, MD- #KatholiekeUniversiteit #MyocardialRepair #Cardiology #Research -Clec4e-Receptor Signaling in My...
Podcast - June-Wha Rhee, MD, FACC @JuneWRhee @StanfordCVI @StanfordMed #AHAJournals #CardioOncology #Cardiology #Onco...
June-Wha Rhee, MD @JuneWRhee @StanfordCVI @StanfordMed #AHAJournals #CardioOncology #Cardiology #Oncology #Research I...
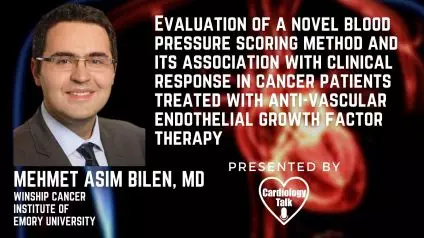
Mehmet Bilen, MD @bilenma @EmoryUniversity @WinshipAtEmory #VEGF #CTCAE #ImmuneRelatedAdverseEvents #Cardiology #Rese...