Bart Meuris, prof. dr. @UZLeuven @HeartValveOrg #Cardiology #Research In-vivo Evaluation Of A Novel Surgical Heart Va...
Bart Meuris, prof. dr. from the University Hospitals Leuven Presentation on the HVS 2021 Abstract In-vivo Evaluation Of A Novel Surgical Heart Valve Prosthesis Designed To Be Durable, Anticoagulant-free And Silent.
Link to Abstract:
https://heartvalvesociety.org/meeting/abstracts/2021/A2.cgi
PURPOSE:
Reoperations of tissue valves or permanent anticoagulation of artificial valves are also drawbacks for heart valve prostheses. The Triflo valve, a tri-leaflet valve made of bio-inert materials with high resistance, was designed to overcome these limitations. In a chronic sheep model, we looked at protection and efficiency.
TECHNIQUES: The Triflo valve (size 21mm) was inserted in two models: in the aortic position for 90 days (n=7) and in the pulmonary position for 70 days (n=4). On-X valves (n=2) were used as a monitor in the pulmonary model. There was no more anticoagulant given after 7 days of low-molecular-weight heparin. Blood tests, echocardiography, acoustic measurements, fluoroscopy, and an autopsy were all performed.
END RESULTS:
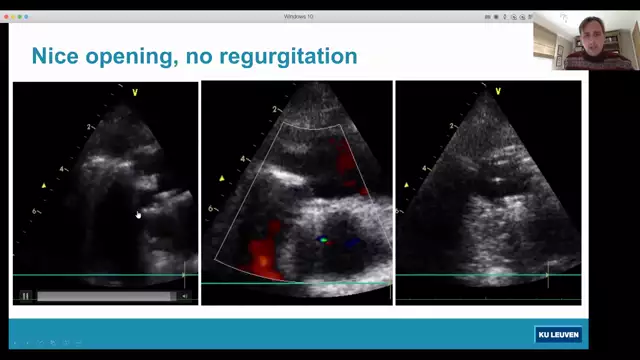
The Triflo valve performed admirably during surgery. In the aortic analysis, there was one aborted surgery and one early death, all unrelated to the prosthesis. All of the other sheep (n=9) recovered well and continued in good clinical condition until they were slaughtered. We found low peak and mean gradients (8.1+/-2.7 and 4.8+/-1.9 mmHg, respectively), a large effective orifice area (2.3+/-0.2 cm2), no valvular regurgitation, and complete left ventricular activity in the aortic role. Both Triflo valves had a smooth surface at explantation, with no valve thrombosis. Thrombo-embolic (TE) damage was not found in any of the main organs. Both valve leaflet mobility was natural in the pulmonary role, and no TE-damage was observed in the lungs. Hematological parameters were stable, and no signs of hemolysis were present. In the pulmonary location, On-X valves performed well, but they produced slightly quieter acoustic signals (p0.05).
RECOMMENDATIONS:
In both the aortic and pulmonary positions, the Triflo valve proved to be safe and reliable. These promising in-vivo effects, which include excellent hemodynamic activity and long-term operation even without anticoagulants, show that this valve is ready for human trials.