Dr. Jung-Joon Cha, MD- Clinical Outcomes in Patients With Delayed Hospitalization for Non–ST-Segment Elevation Myoc...
Dr. Jung-Joon Cha is currently works at the Korea University Anam Hospital, Korea University College of Medicine, in the Division of Cardiology, Department of Internal Medicine. Jung-Joon does research in the fields of interventional cardiology, internal medicine, and translational medicine. In this video, Dr. Cha discusses Clinical Outcomes in Patients With Delayed Hospitalization for Non–ST-Segment Elevation Myocardial Infarction.
https://www.jacc.org/doi/10.1016/j.jacc.2021.11.019
Abstract-
The frequency of patients presenting with non–ST-segment elevation myocardial infarction (NSTEMI) has decreased recently, although there has been an increase in mortality. Prehospital delay due to patients' reluctance to report their symptoms is a likely explanation for increased mortality.
Objectives
The goal of this study was to see if there was a link between prehospital delay and clinical outcomes in NSTEMI patients.
Methods
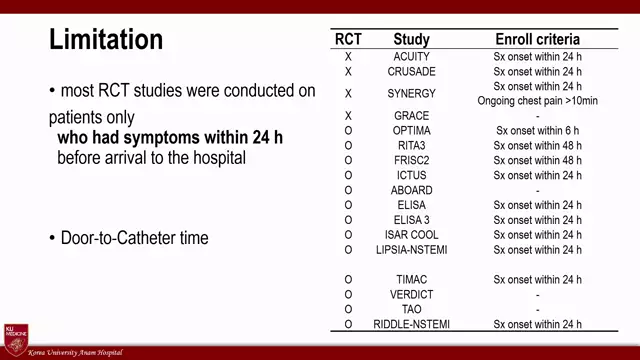
The authors looked at 6,544 patients with NSTEMI out of 13,104 patients from the Korea-Acute-Myocardial-Infarction-Registry–National Institutes of Health. Patients were divided into two groups based on the time from symptom to door (StD) (24 or 24 hours). The primary outcome was all-cause death after three years, while the secondary outcome was a three-year composite of all-cause mortality, recurrent MI, and heart failure hospitalization.
Results
In total, 1,827 patients (27.9%) were assigned to the StD time 24 hours group. The StD time 24 hours group had greater all-cause mortality (17.0 percent vs 10.5 percent; P 0.001) and secondary outcome incidence (23.3 percent vs 15.7 percent; P 0.001). Age, sex, atypical chest pain, dyspnea, Q-wave in electrocardiogram, use of emergency medical services, hypertension, diabetes mellitus, chronic kidney disease, left ventricle dysfunction, TIMI (Thrombolysis In Myocardial Infarction) flow, and the GRACE risk score all showed a higher all-cause mortality in the StD time 24 hours group. The elderly, women, nonspecific symptoms such as atypical chest discomfort or dyspnea, diabetes, and no use of emergency medical services were all independent predictors of prehospital delay in the multivariable analysis.
Conclusions
In patients with NSTEMI, prehospital delay is linked to an increased risk of 3-year all-cause mortality. (C110016) (iCReaT Study No.)